Originally published on Stuff
By Hannah Martin
- A young woman says her life has changed after surgery to treat stage 4 endometriosis.
- Endometriosis is a common condition in which tissue similar to the lining of the uterus grows outside the uterus, which can cause severe pain.
- It’s estimated to affect roughly 1 in every 10 girls, women, and those assigned female at birth.
From her first period at 13, Te Kura Parsons-Grace knew something wasn’t right: she could be “crying” in pain so bad it would cause her to faint.
But for years she says it was regarded as normal. It was “a bit of a mind game — you start to think you’re crazy”, the aspiring primary school teacher said.
So she pushed through. Until one day, curled over in pain at work thinking her appendix may have burst, she says she went to an emergency department.
A diagnostic laparoscopy discovered it wasn’t in the now 26-year-old’s head at all: she had severe stage 4 endometriosis.
Endometriosis is an often painful condition, where tissue similar to the lining of the uterus grows outside the uterus.
Symptoms can include pain with periods; bowel problems such as bloating, diarrhoea, constipation, and pain with bowel movements; painful sexual intercourse; tiredness and low energy; and sub-fertility or infertility, among others.
It’s estimated to affect 120,000 people in Aotearoa — roughly 1 in 10 girls, women and those assigned female at birth, of reproductive age.

SUPPLIED / STUFF
Parsons-Grace said she was “completely riddled” with endometriosis.
In stage 4 endometriosis, the disease affects many pelvic organs, and can often cause distortion of the anatomy and adhesions, according to Endometriosis New Zealand.
On February 1, 2024, Parsons-Grace underwent surgery to excise her endometriosis, which she said has been nothing short of “life-changing”.
Previously, the Tauranga woman’s pain was so “intense” at times she wondered if she’d be able to continue with her studies.
“Some days [I was] not even able to get out of bed.”
Less than 12 weeks on, she feels like a weight has been lifted off her shoulders.

SUPPLIED
Given how common endometriosis is, Parsons-Grace thought better awareness of the chronic pain it causes, and better support, was needed.
Internationally, there was a delay of eight or more years from the time a person first presents to a doctor with symptoms, to diagnosis, according to Endometriosis New Zealand (ENZ).
They say a delay may occur for a number of reasons, including people thinking symptoms are ‘normal’, delaying seeking doctors’ advice, or facing barriers in doing so.
Doctors not recognising the symptoms, misdiagnosing it, or delaying referral to specialist gynaecologists were other potential barriers, ENZ says.
Parsons-Grace was determined to highlight the difficulties faced by people with endometriosis, in the hope that greater awareness will eventually see better support and resources for fellow wāhine.
She also hoped her story offered reassurance and encouragement to others.
A year ago, the thought of even walking up Mauao (Mount Maunganui) was “daunting”, due to the pain she was in.
But during March, Parsons-Grace walked 120 kilometres up and around Mt Maunganui, and bungee-jumped 120m, to raise awareness and funds ‒ a challenge she likened to her overall journey.
“It’s so hard getting to the top, but it’s so amazing being there, knowing where I’d been before.”
President of the The Royal Australian and New Zealand College of Obstetricians and Gynaecologists, Dr Gillian Gibson said endometriosis is a potentially “very debilitating” condition, which can significantly impact quality of life.
Gibson encouraged people struggling with period pain and other symptoms to see their GP early, given there can be a delay in diagnosis, and for GPs to be “enabled and empowered” to make these diagnoses.
Gibson said many gynaecological services were under pressure, and “still catching up” from knock-on effects from Covid-19.
Recent data shows that gynaecology is among specialities with the highest number of people waiting longer than the four-month target for a specialist appointment, as of January.
Thousands waiting longer than target to see a specialist
The number of New Zealanders waiting more than four months for their first specialist appointment, as of January 2024.
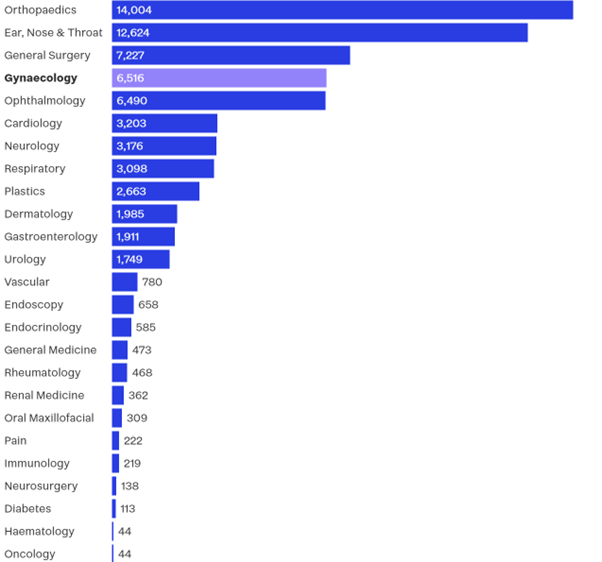
Chart: Sapeer Mayron and Hannah Martin Source: Health New Zealand
Health New Zealand interim national chief medical officer, Nick Baker acknowledged the distress current wait times may be having on women awaiting treatment.
Health services continue to experience “significant pressures” due to sustained high levels of acute demand and workforce shortages, impacting planned care.
The “immediate focus” was on urgent patients and those waiting the longest, and work continued to put processes and systems in place to improve waiting times, Baker said.
In 2020, best practice guidance around the diagnosis and management of endometriosis in New Zealand was published, developed by a taskforce comprising health colleges and those living with endometriosis.
Generally, the guidance aimed to support early recognition of symptoms and empower primary health care practitioners to make a diagnosis and begin management.
And last year, New Zealand published its first Women’s Health strategy.
A priority area of the strategy focused on improving health issues including gynaecological conditions such as endometriosis and pelvic pain, the Ministry of Health’s Emma Prestidge said.
It set directions to health entities around prioritising health research on “women-specific” issues across prevention, screening and treatment; supporting the health workforce to increase their knowledge of such issues; and ensuring there are high-quality, accessible services available.
– Stuff – From dealing with pain for half her life, to a fresh start | Stuff