A health issue is too big to ignore – you’ve come to the right place.
Endometriosis is a common inflammatory disease estimated to affect 176 million individuals worldwide in their reproductive years, and 120,000 in New Zealand. This means that roughly 1 in 10 girls, women and those assigned female at birth in New Zealand will have endometriosis. In most cases, there can be symptoms including period pain, pelvic pain and sub-fertility or infertility. In other cases, there may be no obvious symptoms and the diagnosis is made during the course of medical procedures for other reasons.
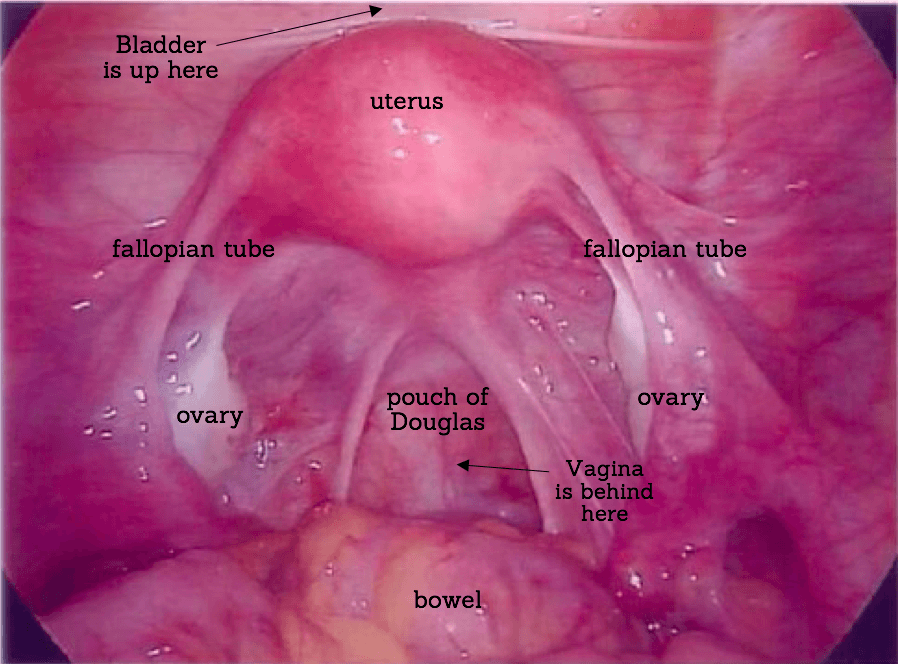
Endometriosis occurs when tissue similar to the lining of the uterus (endometrium), is found in places outside of the uterus. The tissue can form nodules or plaques which may be visualised at surgery. Endometriosis is commonly found in the pelvic region on the thin pelvic lining called the peritoneum. It may be also be found on the pelvic ligaments, ovaries and bowel. Endometriosis is occasionally found in places outside the pelvis such as in scar tissue, the bellybutton or lungs.
Often if you see your doctor with concern about your periods they will order an ultrasound scan. This can not diagnose most forms of endometriosis, but it can pick up cysts on the ovaries (endometrioma).
Endometriosis is commonly associated with adhesions, which can make surgery more challenging.
If there is endometrial tissue in the muscle of the uterus we call it adenomyosis.in the pelvic cavity.
Mild or stage II endometriosis: more extensive than stage I but infiltration of pelvic organs still very limited, without a great deal of scarring or adhesions.
Moderate or stage III endometriosis: sometimes more widespread and starting to infiltrate pelvic organs, peritoneum (pelvic side walls) or other structures. Sometimes there is also scarring and adhesions.
Severe or stage IV endometriosis: infiltrative and affecting many pelvic organs and ovaries, often with distortion of the anatomy and adhesions.

Stages of Endometriosis
Endometriosis is often classified as minimal, mild, moderate or severe or recorded in surgical notes as stage I – IV. This endometriosis staging system is internationally recognised and was established by the ASRM (American Society of Reproductive Medicine).
Here is a brief overview of what the stages mean:
This system provides a useful tool to describe the extent of endometriosis. But, it has limitations. For instance, the extent of endometriosis is not generally related to the symptoms someone experiences. Minimal or mild endometriosis can have symptoms that interfere with the quality of life and likewise, severe endometriosis may not. For this and other reasons, the staging of endometriosis is being investigated and more research is underway to improve how we describe the clinical severity and impact of the disease. Sometimes deep endometriosis is described as deeply infiltrating endometriosis (DIE).
We are hopeful that many more endometriosis surgeons will use not only the revised ASRM classification system, but also when appropriate, the newer Enzian classification for deep endometriosis and the EFI (Endometriosis Fertility index) for people who are concerned about their future fertility. This will help to better understand the extent and likely impact of their disease following laparoscopic surgery.
What Causes Endometriosis
The cause of endometriosis is not fully understood though there are several strong theories. Intensive and extensive research around genetics, immunological and environmental factors continue and further research exploring a range of potential causes and contributing factors is being investigated. The cause is now generally considered multi-factorial with a strong genetic link, possibly also how genetics behave with other influences (perhaps by environmental factors for example).
Endometriosis seems to run in families, so you are more likely to have it if there is a family history. It is important to remember not everyone who has had symptoms will have been diagnosed, but they may have experienced the symptoms.
Symptoms of Endometriosis
Pain during sexual intercourse or afterwards can be common. Internal examination and/or cervical smear can also be painful.
Endometriosis can cause some people to have trouble conceiving which is called sub-fertility. Surgery to remove the endometriosis and restore normal anatomy generally helps fertility. Some people need help to conceive through ART (Assisted Reproductive Technology like IVF).
Discuss all your symptoms with your health professional as it helps with treatment and management. The chronic nature of endometriosis and associated symptoms can be difficult to cope with and can affect relationships, work productivity and general wellbeing.
How is endometriosis diagnosed?
At Endometriosis New Zealand, we understand that receiving a diagnosis can take time and that the process can be frustrating and have a huge impact on many areas of life. You’re not alone, support is available throughout your journey to diagnosis and beyond.
There is currently no simple screening test, such as a blood test, to diagnose endometriosis. Diagnosis often begins with a detailed discussion about symptoms, their impact on daily life, and a physical examination.
Your health practitioner may perform a clinical pelvic examination as part of an initial assessment to investigate suspected endometriosis and to screen for other possible causes of symptoms. A normal clinical examination does not rule out the diagnosis of endometriosis.
Ultrasound
An ultrasound scan can be used to help assess possible endometriosis. A transvaginal ultrasound (internal approach through the vagina) is often the most effective method, but if this is not appropriate, an ultrasound scan through the abdominal wall may be an option (although less precise). An additional specialist ultrasound may be required and should be performed and/or interpreted by a healthcare professional with specialist expertise in gynaecological imaging. However, a normal ultrasound result does not necessarily mean that endometriosis is not present.
MRI
A pelvic MRI can be organised if pelvic ultrasound is not appropriate or if further investigation is needed. MRI can also be useful for identifying areas of concern, but it may be expensive and not always readily available.
Laparoscopy
A laparoscopy is a minimally invasive (“keyhole”) surgical procedure used to diagnose and treat endometriosis. The procedure is done under general anaesthetic (you are asleep) and involves inserting a small camera-equipped tube (laparoscope) through a tiny surgical incision. It is best carried out by a gynaecologist with expertise in treating endometriosis. During surgery, any endometriosis found should be removed and sent to a laboratory for confirmation through histology (microscopic examination).
Laparoscopy is the most reliable way to diagnose endometriosis. Knowing whether you have this condition can help you and your doctor understand your pain, and can also support decisions about fertility planning and long-term management.
Evolving Guidelines and Best Practice
Approaches to diagnosis and treatment are evolving. The Australian Living Evidence Guideline (2025), and other international guidelines emphasise the importance of timely diagnosis through a combination of clinical assessment, non-invasive imaging, and, where indicated, laparoscopy.
This global shift towards non-surgical diagnosis aims to reduce delays, waitlists, and healthcare costs. However, it also highlights the need for greater investment in New Zealand’s diagnostic capacity — including improved access to high-quality ultrasound and MRI equipment, and increased training and support for healthcare professionals in advanced gynaecological imaging. Building workforce capability and ensuring equitable access to these diagnostic services across the country are essential to achieving earlier diagnosis and better outcomes for people with endometriosis.
Similarly, while surgery remains an important option for confirmed or severe cases, these guidelines encourage a more conservative, multidisciplinary approach-reserving surgery for when symptoms and imaging clearly indicate a need. This reduces unnecessary procedures and ensures that patients receive comprehensive and multidisciplinary treatment.
Why is there a delay in diagnosis?
When girls, women and those assigned female at birth…
When doctors…
When gynaecologists…
When others…